Revista Iberoamericana de Neuropsicología
Vol. 1, No. 1, enero-junio 2018.
Family matters in neurorehabilitation: why, when, who, and how?
Anne Norup, PhD11
1 Department of Neurology, Rigshospitalet, Copenhagen University Hospital, Copenhagen, Denmark
Corresponding author:
Anne Norup, PhD.
Department of Neurology,
Rigshospitalet,
Copenhagen University Hospital,
Copenhagen, Denmark.
Email: anne.norup@regionh.dk
Family matters in neurorehabilitation: why, when, who, and how?
The objective of this clinical paper is to describe the different types of family matters that professionals deal with every day when working in rehabilitation. This paper emphasizes WHY and WHEN it is important to work with the whole family and summarizes family reactions throughout the rehabilitation process. Furthermore, it is examined WHO in the family is more at risk of poor caregiver outcomes. Lastly, the paper identifies the needs of the family following brain injury and HOW it is possible to work with the family throughout the different phases of rehabilitation.
During the last few decades, neurorehabilitation after injury to the brain has been accepted as both an appropriate and necessary practice due to its significant impact on everyday life. Acquired brain injury (ABI) is defined as brain injury caused by an event occurring after birth, which is not hereditary, congenital or degenerative(1,2). ABI comprises brain injury with different etiologies such as stroke, traumatic brain injury (TBI), tumors, encephalitis etc., all of which incur a number of consequences within different areas such as physical deficits, cognitive sequela and psychological changes(3). Furthermore, many of the effects are long lasting, causing barriers to participation and independent living. This often requires family members to provide care, supervision and coordination of the neurorehabilitation process(4). In many cases, ABI has chronic consequences, which result in lifestyle changes for the whole family and not just the individual suffering from the brain injury.
The purpose of this paper is to describe the different types of family matters in neurorehabilitation that we as professionals deal with on a daily basis. The paper is based on studies conducted within the field of brain injury as well as clinical experience. Consequently, this paper is not an extensive or systematic review of the literature but a clinical paper providing an overview of relevant studies judged as such by the author. The paper is divided into sections concerning why it is necessary and important to address family matters in neurorehabilitation and secondly, when in the process of neurorehabilitation working with the family is of particular importance, including family reactions during the process. The third part of the paper concerns who in the family is more at risk of developing poor caregiver outcome, and lastly, the paper discusses how to work with the family in the different phases of rehabilitation.
WHY- why does family matter in neurorehabilitation?
ABI can affect anybody at any time. The distribution of etiologies might be different across countries, but an overarching similarity for all types of injuries is that the impact is sudden and immediate, and consequently not expected by the family. Due to the unexpected nature of the injury, the family is not prepared(5). The injury can disrupt the family system and dynamic, eventually leading to poor family functioning(6). The injury causes immediate uncertainty about the future, i.e. “Will she survive the acute phase?” as well as more long-lasting uncertainty as rehabilitation progresses, i.e. “Will he be able to live at home?” or “Will he be able to hold a job?” Consequently, the uncertainty will most likely remain for years to come and will not disappear after the acute treatment.
After the initial acute treatment, deficits in many different areas of function will start to emerge as the patient regains consciousness. An injury to the brain can cause cognitive deficits, physical deficits, and social and behavioral changes as well as changes in emotion and personality, many of which have long-lasting effects. Many studies have assessed and reported on poor psychosocial outcomes among caregivers after ABI. Family members of patients with brain injury are at greater risk of symptoms of anxiety and depression(7-19), post-traumatic stress symptoms(20), increased distress and burden(16,21-29), and diminished life satisfaction(29,30) and quality of life(18,31-35).
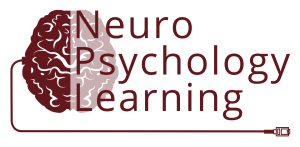
Substantial amounts of literature have emphasized how families and caregivers are affected by the brain injury, resulting in poor mental and physical health. The poor health of the caregivers affects the quality of the care they provide, which affects the outcomes of the patient with the injury. This enhances the risk of social isolation and ultimately, the loss of financial support. This will once again lead to a changed life situation possibly affecting the caregiver’s health. This process can be described as a self-reinforcing circle (Figure 1).
Note: ABI: acquired brain injury. This conceptual model describes some of the factors related to the reciprocal relationship between patient and caregiver outcome. The figure is not a comprehensive description of all the complex interactions between the different factors, but an overview of how these factors are related and affects one another.
This circle increases the risk of long-term mental health problems, which can result in sick leave for the caregiver and a resultant loss of financial resources for the family. Without intervention this self-reinforcing circle can continue indefinitely.
Summing up: Family members become informal caregivers and are an important part of the treatment and rehabilitation process. Thus they do function as an extension of the health care system and will often be the ones who provide the long-term care, support and supervision of the patient(36). The family is an essential key in the reintegration process following rehabilitation, which necessitates making the family a part of the rehabilitation process(36). The family knows the patient best and therefore represents a very important resource during and after the rehabilitation process. Clearly, the family is more than an ‘add-on’.
WHEN does family matter?
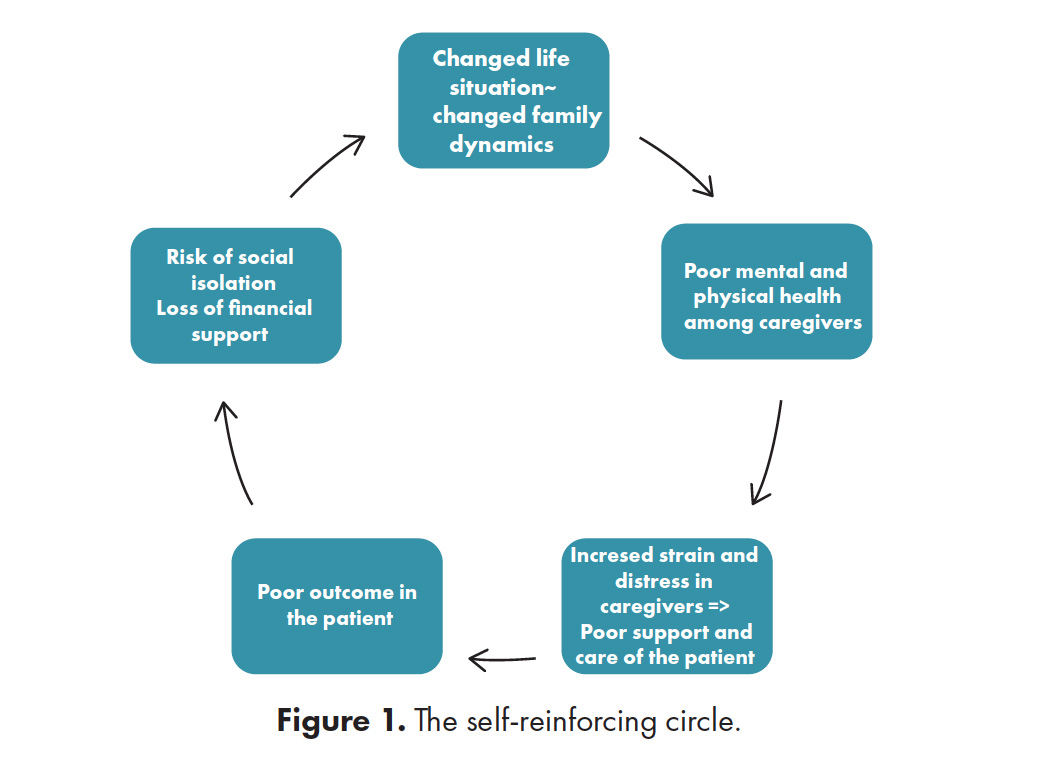
In order to describe family matters occurring in the process of rehabilitation, it is necessary to describe family reactions throughout the rehabilitation process. The phases of rehabilitation are different across countries(37,38), so the proposed model here should be considered generic.
Phase one in the depicted model consists of the acute treatment and care in a hospital, most often in neuro-intensive care unit or regular intensive care. Phase two is rehabilitation in a hospital, where duration can depend on the specific health care system or insurance and can differ significantly across countries. Phase three is rehabilitation outside a hospital, which can be both in-patient and outpatient depending on the need of the patient. Phase four is considered chronic phase consisting of further rehabilitation or maintenance training, if any (Figure 2).
Murial Lezak was one of the first in the brain injury literature to describe the process of family reactions throughout the rehabilitation process(39). She described specific family reactions seen at different time points throughout rehabilitation phases. This description was linear, outlining how the patient progressed simultaneously with the process of the family and how the different reactions followed one another in phases. According to the model, the reactions within the family evolve from initial happiness due to the survival of the patient to mourning and reorganization from 15 months and onward(39).
This is in opposition to a later model proposed by Stroebe & Schut(40). The dual model of coping with bereavement was originally developed to create a framework for dealing with grief after the loss of a loved one(40). However, the dynamic process described in the model can easily be adapted to the caregiving framework. Families living with brain injury do experience loss in terms of loss of function and abilities. The dynamic process described by the dual model fits very well with the clinical experience when working with families who go back and forth between dealing with the loss and orienting themselves for restoration of function. In this way, the coping process is dynamic and oscillatory, as the family sometimes confronts and sometimes avoids the painful situation associated with the loss(40). Coping with the life changes and losses that the brain injury has brought on should include adaptive strategies such as confrontation and avoidance in relation to the losses and restoration.
As mentioned above, a substantial amount of cross-sectional studies have assessed how brain injury affects the wellbeing of the caregivers and immediate family, and these have indicated immediate reactions such as post-traumatic stress(20) and high frequencies of anxiety and depression in the acute phase(18). During rehabilitation and after discharge, high frequencies of both symptoms of depression and anxiety have also been reported(8,9,13,34,41-44), as well as high levels of strain and distress(30,45-47). Decreased quality of life is also a well-known phenomenon during rehabilitation(31,32,34), and at follow-ups many years after injury(33,35,48).
All these cross-sectional studies have provided useful information about the emotional condition of the informal caregivers or close family members at different time points after injury. The innate problem with these studies is that they do not provide any information about changes over time or the direction of causality. It is highly important to know how the emotional condition of the caregivers develops over time and longitudinal studies are needed in order to elucidate the effects of ABI on the family over time. However, only few longitudinal studies have been conducted examining the long-term consequences of ABI on the family and caregivers. Studies examining depression and anxiety over time have found that the amount and severity of symptoms do decrease indicating that even though these families experience severe distress, they are able to manage, adapt and cope over time(49-54). One study has also pointed to the fact that HRQoL increases during the first year after the injury but remains significantly lower when compared to a reference population(55).
In a study conducted in the chronic phase 3 to 6 years after injury assessing caregiver burden and family needs, many of the family caregivers reported unmet needs and increased caregiver burden(21,56). Furthermore, many provided comments about their situation on the reverse side of the questionnaires, indicating how their experiences were still distressing and straining. A wife of a patient, who was living at a nursing home after a severe traumatic brain injury, reported the following:
….what I find most difficult is getting the different persons helping my husband to understand what his brain injury means……….I’m feeling worn out now after 6 years, where there has been different episodes at the nursing home… (they forget to give him the call button, put him in a wheelchair that can’t drive etc.) The problem is that you can’t see the brain injury…..
Wife, 73 yrs.
Another wife of a patient, who lived at home, reported the following:
…… he has no friends and wants me around all the time. Family and kids don’t work –only me. He is very jealous of everything and everybody I talk to or help. I have to be there all the time and live my life the way he wants: very selfish and self-satisfying…..
Wife, 63 yrs
These quotes emphasize how the burden of caregiving does not disappear with time nor diminishes regardless if the patient stays at home or at a caretaking unit. This is also supported by studies indicating how the burden increases from one to two years post injury among caregivers of patients with severe TBI(29).
Summing up: The evidence points to a decrease in symptoms of anxiety and depression during the first year after the patients’ injury. Quality of life increases during the first year, but still does not reach a level comparable to the reference population. Significant caregiver burden has been reported years after injury, and this burden seems to be sustained over time at least in some families. So, does this mean that some families are more at risk of poor outcomes?
Some families cope well with their new life situation, whereas some struggle much more. This has led researchers to investigate and identify caregivers and families who potentially will have poor outcomes. Identification will enable clinicians to target the most vulnerable families for interventions. Many different factors have been investigated such as the influence of social support, age of the patient, severity of injury, and the patient’s level of function or consciousness. The following paragraph briefly summaries some of the factors that studies have identified as related to caregiver outcomes.
Caregiver gender: Some studies have indicated that female caregivers report more symptoms of post-traumatic stress(20), greater strain(54) and higher levels of anxiety and depression(8,18,57). In contrast, Gervasio and colleagues found that male caregivers displayed more distress(10), and this was supported by Perlesz and colleagues who stated that male relatives reported their distress in term of anger and fatigue, whereas female relatives might report their distress in terms of anxiety and depression(16). Some studies have not found any difference between the reporting of male vs. female caregivers in relation to depression(58) or strain(45), and different results have been found in terms of the effect of gender. Due to the unequal distribution of gender in the samples, uncertainties remain when investigating the issue. Qualitative studies might shed light on the different subjective experiences of male and female caregivers.
Relationship: Early studies reported a larger frequency of wives experiencing depression compared to mothers of patients with ABI(59). This finding has also been reported later in relation to depression, anxiety, stress and quality of life(57,60,61), but in contrast to these findings, no differences have also been reported in several other studies(18,20,53,62-64). A review compared experiences of spouses and parents and found that only three out of 16 reviewed papers actually found that TBI had a more negative impact on spouses than other types of caregivers(65). Furthermore, a qualitative study identified a number of subthemes that were different from spouses and parents in relation to the caregiver role(66). Consequently, the needs of parents and spousal caregivers may differ.
Coping style and personality: The use of specific coping strategies seems to be linked to caregiver outcomes. Emotion-focused coping strategies seem to be associated with increased stress and burden, whereas problem-focused coping seems to be associated with lower levels of distress(67-71). In other fields within neurorehabilitation, some research has been conducted in relation to the personality of the caregiver, but this issue has not been explored thoroughly within brain injury literature. In a recent study, we assessed the effect of caregiver personality on outcome and found that caregivers with low neuroticism improved more quickly in symptoms of both anxiety and depression, indicating a more accelerated decrease in anxiety and depression. Even though this study had a small sample size (n=22), it did identify the personality trait neuroticism as a predictor of caregiver outcome(72). Both personality and coping style have been identified as measures relevant to caregiver outcome, but uncertainties remain about the specific effects and longitudinal studies are needed.
Neurobehavioral disturbances. Many of the deficits following brain injury are not visible to others, which makes coping and adjusting especially challenging for both the patient and the surrounding family(4). One consequence of brain injury can be personality change, which is often reported to be particularly debilitating for the family. Anecdotally, personality change after brain injury is described in the literature(73,74) and often observed in clinical practice. However, little research has investigated the frequency and extent of personality changes after brain injury. Several articles have described post-injury personality changes(73-75), but few have investigated personality change using objective and valid personality measures. Only a few studies have been identified that actually compared pre- and post-morbid personality after brain injury(75-77), and only one study has actually investigated how objectively reported personality change affects caregiver mental health without finding a significant association(78).
Summing up. There does seem to be some indication that traits related to the caregiver affects outcomes such as coping style and personality. There seems to be less evidence of relationship being important, at least in relation to anxiety and depression. Few studies have investigated personality change after ABI, as it is difficult to measure, and more research is needed to establish the effect of such changes on caregiver outcomes.
HOW – can we as professionals deal with family matters in neurorehabilitation?
There are no evidence-based guidelines for working with and supporting families living with the consequences of brain injury. One way of dealing with family matters in rehabilitation is to identify the needs of the family, as unmet needs are associated with poorer outcomes in relation to depression(79) and burden(21). It is expected that meeting the needs of families will promote better adaptation to the injury-related sequela of the patient and thereby improve outcome of the caregiver (cf. the self-reinforcing circle).
Studies have tried to identify the needs of the family throughout the rehabilitation process (Figure 2), as these might change over time(80,81). Needs have been identified in both qualitative and quantitative studies at different time points, and some of the main findings from these studies are briefly mentioned here(56,80-82). In phase one, information is important as well as being involved in the care(82). Moreover, maintaining hope and being involved in decision-making is essential for the immediate family members in the acute phase(82). Addressing emotional issues and having a support group is important in both phase one and two(80). Community integration, coordination of care and life planning are described as influential in phase three(80).
One striking thing is that information seems to continue to be important throughout all the phases of rehabilitation, so the need for information continues to be a critical factor, even in the chronic phase three to six years after injury(56). It is more than likely that experiences with caregiving and caregiver needs may differ across healthcare systems, countries and culture. Nevertheless, some global needs have been identified as similar across countries. The importance of health information, professional support and involvement with care needs among families following brain injury were reported across countries(83).
Summing up. The families of brain injury survivors have needs that persist over time and are evident in the chronic phase after brain injury, indicating the need for interventions(56). Such interventions might differ over time and according to the needs of the family. This next paragraph will go through some of the approaches to family interventions in the different phases of rehabilitation.
Phase 1 – acute care: A review concerning the emotional condition of relatives of critically ill patients in intensive care units found that most relatives needed “to have questions answered honestly” and “to know specific facts regarding what is wrong with the patient and the patient’s progress”. The review concluded that information was the most important need identified in critical care when the patients’ situation is unstable. The families sought honest and frequent information about progress, status and prognosis(84).
Marks & Daggett developed a pathway for meeting the needs of families of patients with severe TBI in the NICU, and the pathway was evaluated by nurses working in acute care. Ultimately, wise assessment and compassionate intervention by nurses and physicians were identified as factors that ensured quality of patient and family care. The use of this critical pathway can help nurses working in the NICU to develop and assess creative interventions to meet the needs of families trying to cope with the effects of TBI.
We conducted a pilot study using a neuropsychological intervention including 46 close family members during acute care following severe brain injury described in detail elsewhere(85). The intervention was conducted by an experienced neuropsychologist, and the specific topics of the sessions depended on the relatives’ needs. Every session began with the neuropsychologist asking the family how they experienced the accident, i.e. if they witnessed it or were involved. In cases in which the relatives had not been present, they were asked to share how they received the message about the accident. The relatives often needed immediate psychological support to help them deal with their own emotional reactions and needs during the first critical phases of the patients’ stay in the acute setting. Topics often addressed in the supportive part of the sessions were how to handle each day with a close family member in a hospital as well as coping with feelings of isolation, guilt and emotional distress. The second part of the sessions was psycho-educational, and the relatives were able to ask any questions regarding treatment in the acute setting including the first period of unconsciousness, post-traumatic amnesia, consequences of brain injury and recovery from brain injury. In some cases, the relatives had obvious symptoms of anxiety, such as being tense, physically restless and almost unable to sit still. In such sessions, the focus remained on the immediate situation and how to handle this. In cases where the families were more calm and able to receive information, the neuropsychologist tried to answer questions about prognosis, treatment in the acute setting etc. It was very important that each session was finished properly, and clinicians made sure that the family members had no further questions or queries.
Phase 2 – hospital rehabilitation: During the hospital stay, the options for psychoeducation and support for families varies a great deal. The following paragraph describes the support provided in a highly specialized unit for severe TBI, consisting of individual sessions with a neuropsychologist and the possible participation in a support group (the details of this support program has been thoroughly described elsewhere; 41). The first individual session is prompted by the neuropsychologist, who contacts the relatives at the patient’s admission. This appointment is primarily aimed at giving relatives information about severe TBI and its possible consequences. The first session is often the beginning of a more supportive psychological process with the relatives. The sessions with the neuropsychologist are psycho-educational as well as supportive. Their content depends on the relatives and their specific needs. Usually the relatives express a need for information about TBI, its possible consequences, and recovery from TBI, including the first period of unconsciousness, post-traumatic amnesia and the following remaining deficits. Furthermore, the relatives often need support to help them deal with their own emotional reactions and needs during the patients’ recovery. Topics often addressed in the supportive part of the sessions are role shifting in the family, mixed feelings about the person with the brain injury, how to handle each day with a close family member in hospital, and feelings of isolation, guilt and emotional distress. The intervention is individualized according to the relatives’ needs and is a flexible mixture of both psycho-education and emotional support. The relatives are offered the opportunity to participate in a support group led by a neuropsychologist, where the relatives can debate topics of their own choice. The neuropsychologist moderates the group, but otherwise the group is not structured. The group starts with an introduction, where the relatives are asked to tell the group what has happened to their family member. However, if a relative merely wants to listen at their first visit, this is also acceptable. The objective of the group is primarily supportive and only educational in the sense that relatives learn about the different types of brain injury and their consequences and recovery when listening to other relatives(41).
Phase 3 to 4 – rehabilitation and maintenance: After discharge from rehabilitation in a hospital, many patients still need further rehabilitation. At this point the family starts adjusting to a more stable situation, as many patients are discharged to their own home depending on their acquired disabilities. At this point, the family will start getting insights in to what their new life situation will be like as changes become more apparent.
The need for support and services offered can vary. Problem-solving training (PST) is one form of intervention that has been tested among caregivers of patients with brain injury. PST aims to solve the problem of the individual caregiver(86), typically combining education to increase knowledge and counseling or therapy to increase the understanding and use of strategies to manage stress and symptoms of depression and anxiety(87). A randomized controlled trial investigated the effect of PST for family caregivers of persons with TBI over a period of 12 months. This trial consisted of four in-home problem-solving training sessions and telephone sessions during the remaining months. Caregivers in the intervention group reported significant reductions in depression, health complaints and dysfunctional problem-solving styles, but no effects were seen on well-being, burden or constructive problem-solving styles(88). Another study used a telehealth-approach to individualized education and PST to caregivers in the general community. The study found that caregivers in the intervention group felt they received more assistance from others, felt more success in gaining information from healthcare providers and were better able to care for themselves(89). This study is one of the first within brain injury to use a telehealth approach. Such approaches have gained attention and interest with the development of technology and can be of particular interest to people living in rural areas.
As far as the author knows, only two approaches have been developed including the whole family: the Brain Injury Family Intervention (BIFI)(90) and Traumatic Brain Injury/Spinal Cord Injury Family Intervention(91). Kreutzer and co-workers have developed the Brain Injury Family Intervention (BIFI): a structured intervention program, which includes educational, skill building and psychological support components(90). The outpatient program consists of five two-hour intervention sessions, and the intervention is conducted by doctoral level psychologists. The benefits of the BIFI program have been reported in different publications. First, a preliminary investigation of 53 caregivers and TBI survivors indicated a greater number of met needs and perception of fewer obstacles to receiving services. However, the program had no effect on standardized measures of psychological distress, family function and life satisfaction(92).
One year later the authors published new results on the program, this time on a larger sample (n=76 survivors and caregivers, however still including the first sample). Outcome measures reported were a Learning Survey, a Session Report Form and Program Satisfaction Survey. The outcome measures were designed to evaluate the different aspects of the program on Likert type scales. Patients and caregivers rated sessions ‘helpfulness,’ in terms of its ability to help them meet their goals, as high. The authors thus concluded that BIFI is perceived as helpful and that the treatment methods may facilitate the achievement of goals(93). A recent study assessing the efficacy of the BIFI found that an intervention group completing the BIFI program reported a greater number of needs met at completion of treatment, which was significant on four of the six subscales of Family Needs Questionnaire(94).
Another family intervention including the whole family is the Traumatic Brain Injury/Spinal Cord Injury Family Intervention(91) developed for use with families living with spinal cord injury or traumatic brain injury. Strategies and elements from cognitive-behavioral and family therapy – including structural family therapy, narrative therapy, and solution focused therapy – were integrated to create a sequence of eight weekly, 90-minute sessions that have educational and practical components related to common experiences reported by families facing brain injury. The content, strategies, and theoretical approach of each of the eight sessions are described elsewhere(91). Each session begins with reflection on a quotation that is relevant to the week’s topic, followed by review of the family’s progress on assigned practice tasks. The majority of each session is devoted to learning background information about the topic, practicing new techniques, and applying those techniques to overcome the unique challenges that each family is facing. Each session ends with a home assignment. Though the intervention is manualized, families can apply the skills from each session to whatever issue or conflict they are facing. The intervention was designed to be conducted in family-specific group sessions that involved both the individual with brain injury and at least two family members. A pilot study among families living with spinal cord injury found preliminary evidence that symptoms of depression, anxiety, and burden as well as problem-solving appraisals improved significantly for individuals who participated in the intervention compared to those in the waitlist control group(91). The intervention has been translated to other languages and is currently being tested in several countries(95).
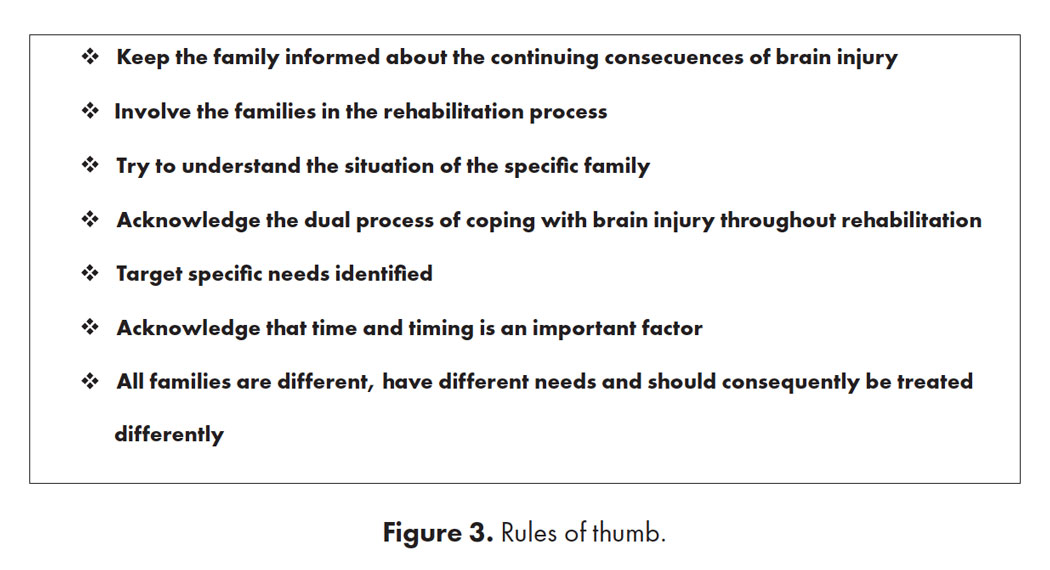
Summing up: Possible interventions have been outlined as well as the importance of providing support to families following brain injury throughout the rehabilitation phases. Furthermore, it is crucial that support are provided long term, as the families’ needs and their readiness to receive it do change. So far, no evidence-based guidelines have been developed, but rules of thumb based on clinical experience and research are presented in Figure 3.
This paper has investigated and discussed the why, when, who and how in relation to working with family matters in neurorehabilitation. In accordance with the research discussed in this paper, it is very likely that the patient indirectly benefits from the support provided to the relatives as it is clear that the mental state of the relative is important to the patients’ care both during the process of rehabilitation and in the future. The symptoms of distress experienced by relatives may have important long-term consequences for the family and the patient with respect to employment and quality of life as illustrated by the self-reinforcing circle. Early detection of symptoms of anxiety and providing necessary support may very well prevent the more long-term symptoms of depression at least to some extent. Symptoms of distress can influence the collaboration between staff working in rehabilitation and the family, which may result in a very stressful work environment for professionals and a negative rehabilitation environment for the family. Common reactions have been described throughout the paper, but no predictable patterns exist as every family and survivor is different and unique. It is important for health care professionals and organizations to have support systems that can adequately meet the needs of the families. Support systems should be based on clinical experience and evidence supported interventions in the different phases of rehabilitation. Health organizations and rehabilitation services should have a structured approach towards supporting the family during and after the patients’ rehabilitation. The support system can feature professionals working in a rehabilitation setting or by providing the relatives with links to other organizations, public or private.
Continuity is important in the process of rehabilitation. Effective strategies linking the different services in the different phases of rehabilitation will very likely relieve caregivers of strain and distress to some extent as the relatives themselves often serve as the continuity during transitional periods. A continuous family-focused approach in rehabilitation may be more effective for both the patient and their family as family matters in successful neurorehabilitation.
I would like to thank Serena Brandler for her language editing, and proofreading of this manuscript.
- DeDios-Stern S, Lee E-J. Blame, Coping, and Psychosocial Outcomes in Caregivers of Individuals With Brain Injury. 2017 Apr 27 [cited 2017 Jun 22]; Available from: http://www.ncbi.nlm.nih.gov/ pubmed/28447806
- Oyesanya T. The experience of patients with ABI and their families during the hospital stay: A systematic review of qualitative literature. Brain Inj [Internet]. 2017 Jan 28 [cited 2017 Jun 22];31(2):151–73. Available from: http://www.ncbi.nlm.nih.gov/pubmed/28055226
- Lishman WA. Organic Psychiatry. Vol. 3rd. Oxford: Blackwell Publishers; 1997.
- Manskow US. Caregivers to patients with severe traumatic brain injury. 2016.
- Sinnakaruppan I, Williams DM. Family carers and the adult head-injured: a critical review of carers’ needs. Brain Inj [Internet]. 2001 Aug;15(8):653–72. Available from: isi:000170452100001
- Schonberger M, Ponsford J, Olver J, Ponsford M. A longitudinal study of family functioning after TBI and relatives’ emotional status. NeuropsycholRehabil. 2010 Dec;20(1464–0694 (Electronic)):813–29.
- Perez-San Gregorio MA, Blanco-Picabia A, Murillo-Cabezas F, Dominguez-Roldan JM, Sanchez B, Nunez-Roldan A. Psychological problems in the family members of gravely traumatised patients admitted into an intensive care unit. Intensive Care Med. 1992;18(0342–4642 (Print)):278–81.
- Linn RT, Allen K, Willer BS. Affective Symptoms in the Chronic Stage of Traumatic Brain Injury – A Study of Married-Couples. Brain Inj [Internet]. 1994 Feb;8(2):135–47. Available from: isi:A1994NA02900003
- Mintz MC, Vanhorn KR, Levine MJ. Developmental Models of Social Cognition in Assessing the Role of Family Stress in Relatives Predictions Following Traumatic Brain Injury. Brain Inj [Internet]. 1995 Feb;9(2):173–86. Available from: isi:A1995QN62800006
- Gervasio AH, Kreutzer JS. Kinship and family members’ psychological distress after traumatic brain injury: A large sample study. J Head Trauma Rehabil [Internet]. 1997 Jun;12(3):14–26. Available from: isi:A1997XC69900003
- Wallace CA, Bogner J, Corrigan JD, Clinchot D, Mysiw WJ, Fugate LP. Primary caregivers of persons with brain injury: life change 1 year after injury. Brain Inj. 1998 Jun;12(0269–9052 (Print)):483–93.
- Douglas JM, Spellacy FJ. Indicators of long-term family functioning following severe traumatic brain injury in adults. Brain Inj. 1996 Nov;10(11):819–39.
- Rivera P, Elliott TR, Berry JW, Grant JS, Oswald K. Predictors of caregiver depression among community-residing families living with traumatic brain injury. NeuroRehabilitation. 2007;22(1):3–8.
- Giovannetti AM, Leonardi M, Pagani M, Sattin D, Raggi A. Burden of caregivers of patients in Vegetative State and Minimally Conscious State. Acta NeurolScand. 2012 Apr 17;(1600–0404 (Electronic)).
- Leonardi M, Giovannetti AM, Pagani M, Raggi A, Sattin D, And OBOTNCFADIV, et al. Burden and needs of 487 caregivers of patients in vegetative state and in minimally conscious state: Results from a national study. Brain Inj. 2012 May 9;(1362–301X (Electronic)).
- Perlesz A, O’Loughlan M. Changes in stress and burden in families seeking therapy following traumatic brain injury: a follow-up study. IntJRehabilRes. 1998 Dec;21(0342–5282 (Print)):339–54.
- Ponsford J, Olver J, Ponsford M, Nelms R. Long-term adjustment of families following traumatic brain injury where comprehensive rehabilitation has been provided. Brain Inj. 2003 Jun;17(6):453–68.
- Norup A, Welling K-L, Qvist J, Siert L, Mortensen EL. Depression, anxiety and quality-of-life among relatives of patients with severe brain injury: The acute phase. Brain Inj. 2012 May 30;26(1362–301X (Electronic)).
- Norup A, Kristensen KS, Poulsen I, Nielsen CL, Mortensen EL. Clinically significant changes in the emotional condition of relatives of patients with severe traumatic brain injury during sub-acute rehabilitation. J Rehabil Med. 2013;45(8):820–6.
- Pielmaier L, Walder B, Rebetez MM, Maercker A. Post-traumatic stress symptoms in relatives in the first weeks after severe traumatic brain injury. Brain Inj. 2011;25(1362–301X (Electronic)):259–65.
- Doser K, Norup A. Caregiver burden in Danish family members of patients with severe brain injury: The chronic phase. Brain Inj [Internet]. 2016;30(3):334–42. Available from: http://ovidsp.ovid.com/ovidweb.cgi?T=JS&PAGE=reference&D=emed13&NEWS=N&AN=20160134556
- Manskow US, Sigurdardottir S, Røe C, Andelic N, Skandsen T, Damsgård E, et al. Factors Affecting Caregiver Burden 1 Year After Severe Traumatic Brain Injury: A Prospective Nationwide Multicenter Study. J Head Trauma Rehabil [Internet]. 2014;30(6):1–13. Available from: http://www.ncbi.nlm.nih. gov/pubmed/25119652
- Elmståhl S, Malmberg B, Annerstedt L. Caregiver’s burden of patients 3 years after stroke assessed by a novel caregiver burden scale. Arch Phys Med Rehabil. 1996;77(2):177–82.
- Marsh N V, Kersel DA, Havill JH, Sleigh JW. Caregiver burden at 1 year following severe traumatic brain injury. Brain Inj. 1998 Dec;12(0269–9052 (Print)):1045–59.
- Katz S, Kravetz S, Grynbaum F. Wives’ coping flexibility, time since husbands’ injury and the perceived burden of wives of men with traumatic brain injury. Brain Inj. 2005 Jan;19(0269–9052 (Print)):59–66.
- Lehan T, Arango-Lasprilla JC, de los Reyes CJ, Quijano MC. The ties that bind: the relationship between caregiver burden and the neuropsychological functioning of TBI survivors. NeuroRehabilitation. 2012;30(1878–6448 (Electronic)):87–95.
- Marsh N V, Kersel DA, Havill JH, Sleigh JW. Caregiver burden at 6 months following severe traumatic brain injury. Brain Inj. 1998 Mar;12(0269–9052 (Print)):225–38.
- Carnevale GJ, Anselmi V, Busichio K, Millis SR. Changes in ratings of caregiver burden following a community-based behavior management program for persons with traumatic brain injury. JHead Trauma Rehabil. 2002 Apr;17(0885–9701 (Print)):83–95.
- Manskow US, Friborg O, Røe C, Braine M, Damsgard E, Anke A. Patterns of change and stability in caregiver burden and life satisfaction from 1 to 2 years after severe traumatic brain injury: A Norwegian longitudinal study. NeuroRehabilitation [Internet]. 2017 Mar 27 [cited 2017 Jun 29];40(2):211–22. Available from: http://www.ncbi.nlm.nih.gov/pubmed/27935561
- Kreutzer JS, Rapport LJ, Marwitz JH, Harrison-Felix C, Hart T, Glenn M, et al. Caregivers’ well-being after traumatic brain injury: a multicenter prospective investigation. ArchPhysMedRehabil. 2009 Jun;90(1532–821X (Electronic)):939–46.
- Arango-Lasprilla JC, Nicholls E, Villasenor CT, Drew A, Jimenez-Maldonado M, Martinez-Cortes ML. Health-related quality of life in caregivers of individuals with traumatic brain injury from Guadalajara, Mexico. JRehabilMed. 2011 Nov;43(1651–2081 (Electronic)):983–6.
- McPherson KM, Pentland B, McNaughton HK. Brain injury – the perceived health of carers. Disabil Rehabil [Internet]. 2000 Oct;22(15):683–9. Available from: isi:000165329300005
- Moules S, Chandler BJ. A study of the health and social needs of carers of traumatically brain injured individuals served by one community rehabilitation team. Brain Inj. 1999 Dec;13(12):983–93.
- Norup A, Siert L, Mortensen EL. Emotional distress and quality of life in relatives of patients with severe brain injury: The first month after injury. Brain Inj. 2010 Feb;24(1362–301X (Electronic)):81–8.
- Vogler J, Klein A-M, Bender A. Long-term health-related quality-of-life in patients with acquired brain injury and their caregivers. Brain Inj [Internet]. 2014 Oct 19 [cited 2017 Jun 28];28(11):1381–8. Available from: http://www.ncbi.nlm.nih.gov/pubmed/24945467
- Ramkumar NA, Elliott TR. Family caregiving of persons following neurotrauma: issues in research, service and policy. NeuroRehabilitation [Internet]. 2010 [cited 2017 Jun 27];27(1):105–12. Available from: http://www.ncbi.nlm.nih.gov/pubmed/20634605
- Engberg AW. A Danish national strategy for treatment and rehabilitation after acquired brain injury. J Head Trauma Rehabil [Internet]. 2007;22(4):221–8. Available from: http://www.ncbi.nlm.nih.gov/pubmed/17667064
- British society of rehabilitation medicine. Rehabilitation following acquired brain injury. National clinical guidelinges. 2003.
- Lezak MD. Psychological Implications of Traumatic Brain Damage for the Patients Family. 1986;31(4):241–50.
- Stroebe M, Schut H. The dual process model of coping with bereavement: rationale and description. Death Stud [Internet]. 1999 Mar [cited 2017 Jun 27];23(3):197–224. Available from: http://www.ncbi.nlm.nih.gov/pubmed/10848151
- Norup A, Kristensen KSKS, Siert L, Poulsen I, Mortensen ELEL. Neuropsychological support to relatives of patients with severe traumatic brain injury in the sub-acute phase. Neuropsychol Rehabil [Internet]. 2011;21(3):306–21. Available from: http://www.ncbi.nlm.nih.gov/pubmed/21452099
- Norup A, Kristensen KS, Poulsen I, Mortensen EL. Evaluating clinically significant changes in health-related quality of life: A sample of relatives of patients with severe traumatic brain injury. Neuropsychol Rehabil. 2015;(August).
- Perlesz A, Kinsella G, Crowe S. Psychological distress and family satisfaction following traumatic brain injury: Injured individuals and their primary, secondary, and tertiary carers. J Head Trauma Rehabil [Internet]. 2000 Jun;15(3):909–29. Available from: isi:000087445400005
- Douglas JM, Spellacy FJ. Correlates of depression in adults with severe traumatic brain injury and their carers. Brain Inj. 2000 Jan;14(0269–9052 (Print)):71–88.
- Boycott N, Yeoman P, Vesey P. Factors Associated With Strain in Carers of People With Traumatic Brain Injury. JHead Trauma Rehabil. 2012 Apr 10;(1550–509X (Electronic)).
- Brooks DN. The head-injured family. J Clin Exp Neuropsychol. 1991;13(1):155–88.
- Kreutzer JS, Gervasio AH, Camplair PS. Patient Correlates of Caregivers Distress and Family Functioning After Traumatic Brain Injury. Brain Inj [Internet]. 1994 Apr;8(3):211–30. Available from: isi:A1994ND71400003
- Koskinen S. Quality of life 10 years after a very severe traumatic brain injury (TBI): the perspective of the injured and the closest relative. Brain Inj [Internet]. 1998 Aug;12(8):631–48. Available from: isi:000075243800001
- Livingston MG, Brooks DN, Bond MR. Patient Outcome in the Year Following Severe Head-Injury and Relatives Psychiatric and Social Functioning. J Neurol Neurosurg Psychiatry [Internet]. 1985;48(9):876–81. Available from: isi:A1985AQS1500005
- Norup A, Petersen J, Mortensen EL. Relatives of patients with severe brain injury: Growth curve analysis of anxiety and depression the first year after injury. Brain Inj. 2015;29(7–8).
- Novack TA, Bergquist TF, Bennett G, Gouvier WD. Primary caregiver distress following severe head injury. J Head Trauma Rehabil. 1991;6(4):69–77.
- Oddy M, Coughlan T, Tyerman A, Jenkins D. Social adjustment after closed head injury: a further follow-up seven years after injury. JNeurolNeurosurgPsychiatry. 1985 Jun;48(0022–3050 (Print)):564–8.
- Oddy M, Humphrey M, Uttley D. Stresses Upon Relatives of Head-Injured Patients. Br J Psychiatry [Internet]. 1978;133(DEC):507–13. Available from: isi:A1978FZ11400004
- Turner B, Fleming J, Parry J, Vromans M, Cornwell P, Gordon C, et al. Caregivers of Adults WTraumatic Brain Injury: The Emotional Impact of Transition From Hospital to Home. Brain Impair [Internet]. 2010 Dec;11(3):281–92. Available from: http://search.ebscohost.com/login.aspx?direct=true&db=a9h&AN=57434494&site=ehost-live
- Norup A, Snipes D, Siert L, ELM, Perrin PB, Arango-Lasprilla JC. Longitudinal trajectories of health related quality of life in Danish family members of individuals with severe brain injury. Aust J Rehabil Couns. 2013;19(2):71–83.
- Doser K, Norup A. Family needs in the chronic phase after severe brain injury in Denmark. Brain Inj. 2014;28(10).
- Norup A, Petersen J, Mortensen EL. Relatives of patients with severe brain injury: Growth curve analysis of anxiety and depression the first year after injury. Brain Inj [Internet]. 2015;29(7–8):822–9. Available from: http://ovidsp.ovid.com/ovidweb.cgi?T=JS&PAGE=reference&D=medl&NEWS=N&AN=25962925
- Harris JK, Godfrey HP, Partridge FM, Knight RG. Caregiver depression following traumatic brain injury (TBI): a consequence of adverse effects on family members? Brain Inj. 2001 Mar;15(3):223–38.
- Mauss-Clum N, Ryan M. Brain injury and the family. J Neurosurg Nurs. 1981 Aug;13(4):165–9.
- Kreutzer JS, Gervasio AH, Camplair PS. Primary Caregivers Psychological Status and Family Functioning After Traumatic Brain Injury. Brain Inj [Internet]. 1994 Apr;8(3):197–210. Available from: isi:A1994ND71400002
- Leathem J, Heath E, Woolley C. Relatives’ perceptions of role change, social support and stress after traumatic brain injury. Brain Inj. 1996 Jan;10(1):27–38.
- Ergh TC, Rapport LJ, Coleman RD, Hanks RA. Predictors of caregiver and family functioning following traumatic brain injury: social support moderates caregiver distress. JHead Trauma Rehabil. 2002 Apr;17(0885–9701 (Print)):155–74.
- Gillen R, Tennen H, Affleck G, Steinpreis R. Distress, depressive symptoms, and depressive disorder among caregivers of patients with brain injury. J Head Trauma Rehabil [Internet]. 1998 Jun;13(3):31–43. Available from: isi:000074042200004
- Knight RG, Devereux R, Godfrey HP. Caring for a family member with a traumatic brain injury. Brain Inj. 1998 Jun;12(0269–9052 (Print)):467–81.
- Ennis N, Rosenbloom BN, Canzian S, Topolovec-Vranic J. Depression and anxiety in parent versus spouse caregivers of adult patients with traumatic brain injury: a systematic review. NeuropsycholRehabil. 2013;23(1464–0694 (Electronic)):1–18.
- Kratz AL, Sander AM, Brickell TA, Lange RT, Carlozzi NE. Traumatic brain injury caregivers: A qualitative analysis of spouse and parent perspectives on quality of life. Neuropsychol Rehabil [Internet]. 2017 Jan 2 [cited 2017 Jul 6];27(1):16–37. Available from: http://www.ncbi.nlm.nih.gov/pubmed/26052805
- Calvete E, de Arroyabe EL. Depression and grief in Spanish family caregivers of people with traumatic brain injury: The roles of social support and coping. Brain Inj. 2012;26(1362–301X (Electronic)):834–43.
- Chronister J, Chan F, Sasson-Gelman EJ, Chiu CY. The association of stress-coping variables to quality of life among caregivers of individuals with traumatic brain injury. NeuroRehabilitation. 2010;27(1878–6448 (Electronic)):49–62.
- Cruzado JA, Elvira de la Morena MJ. Coping and distress in caregivers of patients with disorders of consciousness. Brain Inj [Internet]. 2013 Jul 30 [cited 2017 Jun 22];27(7–8):793–8. Available from: http://www.ncbi.nlm.nih.gov/pubmed/23631550
- Norup A, Siert L, Lykke Mortensen E. Coping strategies, emotional distress and quality of life in relatives of pateints with severe brain injury in Denmark: One year after injury. Aust J Rehabil Couns. 2013;19(2):142–54.
- Sander AM, High Jr. WM, Hannay HJ, Sherer M. Predictors of psychological health in caregivers of patients with closed head injury. Brain Inj. 1997 Apr;11(0269–9052 (Print)):235–49.
- Trujillo M, Perrin PB, Doser K, Norup A. Using Personality Traits to Construct Linear Growth Models of Mental Health in Family Members of Individuals With Severe Brain Injury. Rehabil Psychol [Internet]. 2016; Available from: https://liverpool.idm.oclc.org/login?url=http://search.ebscohost.com/login.aspx?direct=true&db=psyh&AN=2016-49571-001&site=ehost-live&scope=site%0AORCID: 0000-0002-5598-6116
- Brooks DN, McKinlay W. Personality and behavioural change after severe blunt head injury–a relative’s view. JNeurolNeurosurgPsychiatry. 1983 Apr;46(4):336–44.
- Lezak MD. Living with the characterologically altered brain injured patient. J Clin Psychiatry. 1978 Jul;39(7):592–8.
- Prigatano GP. Personality disturbances associated with traumatic brain injury. J Consult Clin Psychol. 1992;60(3):360–8.
- Tate RL. Impact of pre-injury factors on outcome after severe traumatic brain injury: Does post-traumatic personality change represent an exacerbation of premorbid traits? Neuropsychol Rehabil [Internet]. 2003 Jan [cited 2017 Aug 15];13(1–2):43–64. Available from: http://www.ncbi.nlm.nih.gov/pubmed/21854327
- Kurtz JE, Putnam SH, Stone C. Stability of normal personality traits after traumatic brain injury. J Head Trauma Rehabil [Internet]. 1998 Jun [cited 2017 Aug 15];13(3):1–14. Available from: http://www.ncbi.nlm.nih.gov/pubmed/9582175
- Norup A, Mortensen EL. Prevalence and predictors of personality change after severe brain injury. Arch Phys Med Rehabil [Internet]. 2015;96(1):56–62. Available from: http://dx.doi.org/10.1016/j.apmr.2014.08.009
- Leibach GG, Trapp SK, Perrin PB, Everhart RS, Cabrera TV, Jimenez-Maldonado M, et al. Family needs and TBI caregiver mental health in Guadalajara, Mexico. NeuroRehabilitation [Internet]. 2014 [cited 2017 Sep 29];34(1):167–75. Available from: http://www.ncbi.nlm.nih.gov/pubmed/24284459
- Rotondi AJ, Sinkule J, Balzer K, Harris J, Moldovan R. A qualitative needs assessment of persons who have experienced traumatic brain injury and their primary family caregivers. J Head Trauma Rehabil [Internet]. 2007 [cited 2017 Jun 22];22(1):14–25. Available from: http://www.ncbi.nlm.nih.gov/pubmed/17235227
- Tverdov AH, McClure KS, Brownsberger MG, Armstrong SL. Family needs at a post-acute rehabilitation setting and suggestions for supports. Brain Inj [Internet]. 2016 Feb 23 [cited 2017 Jun 22];30(3):324–33. Available from: http://www.tandfonline.com/doi/full/10.3109/02699052.2015.1113566
- Wetzig K, Mitchell M. The needs of families of ICU trauma patients: an integrative review. Intensive Crit Care Nurs [Internet]. 2017 Aug [cited 2017 Jun 29];41:63–70. Available from: http://www.ncbi.nlm.nih.gov/pubmed/28366520
- Norup A, Perrin PB, Cuberos-Urbano G, Anke A, Andelic N, Doyle ST, et al. Family needs after brain injury: A cross cultural study. NeuroRehabilitation. 2015;36(2):203–14.
- Hickey M. What are the needs of families of critically ill patients? A review of the literature since 1976. Hear Lung. 1990 Jul;19(0147–9563 (Print)):401–15.
- Norup A, Siert L, Mortensen EL. Neuropsychological intervention in the acute phase: A pilot study of emotional wellbeing of relatives of patients with severe brain injury. J Rehabil Med. 2013;45(8):827–34.
- Rivera PA, Elliott TR, Berry JW, Grant JS. Problem-solving training for family caregivers of persons with traumatic brain injuries: a randomized controlled trial. Arch Phys Med Rehabil [Internet]. 2008 May [cited 2017 Sep 18];89(5):931–41. Available from: http://www.ncbi.nlm.nih.gov/pubmed/18452743
- Boschen K, Gargaro J, Gan C, Gerber G, Brandys C. Family interventions after acquired brain injury and other chronic conditions: a critical appraisal of the quality of the evidence. Neuro Rehabilitation [Internet]. 2007 [cited 2017 Jun 28];22(1):19–41. Available from: http://www.ncbi.nlm.nih.gov/pubmed/17379946
- Rivera PA, Elliott TR, Berry JW, Grant JS. Problem-solving training for family caregivers of persons with traumatic brain injuries: a randomized controlled trial. ArchPhysMedRehabil. 2008 May;89(1532–821X (Electronic)):931–41.
- Powell JM, Fraser R, Brockway JA, Temkin N, Bell KR. A Telehealth Approach to Caregiver Self-Management Following Traumatic Brain Injury. J Head Trauma Rehabil [Internet]. 2016 [cited 2017 Sep 14];31(3):180–90. Available from: http://www.ncbi.nlm.nih.gov/pubmed/26394294
- Kreutzer JS, Kolakowsky-Hayner SA, Demm SR, Meade MA. A structured approach to family intervention after brain injury. JHead Trauma Rehabil. 2002 Aug;17(0885–9701 (Print)):349–67.
- Lehan T, Stevens LF, Arango-Lasprilla JC. Traumatic Brain Injury (TBI)/Spinal Cord Injury (SCI) Family Intervention. Top Spinal Cord Inj Rehabil. 2016;22(1):Suppl.
- Kreutzer JS, Stejskal TM, Ketchum JM, Marwitz JH, Taylor LA, Menzel JC. A preliminary investigation of the brain injury family intervention: impact on family members. Brain Inj. 2009 Jun;23(1362–301X (Electronic)):535–47.
- Kreutzer JS, Stejskal TM, Godwin EE, Powell VD, Arango-Lasprilla JC. A mixed methods evaluation of the Brain Injury Family Intervention. NeuroRehabilitation. 2010;27(1878–6448 (Electronic)):19–29.
- Kreutzer JS, Marwitz JH, Sima AP, Godwin EE. Efficacy of the Brain Injury Family Intervention. J Head Trauma Rehabil [Internet]. 2015 [cited 2017 Sep 14];30(4):249–60. Available from: http://www.ncbi.nlm.nih.gov/pubmed/26147315
95. Rasmussen MS, Andelic N, Nordenmark T, Arango-Lasprilla JC, Soberg H. Family as a Resource for Improved Patient and Family Functioning After Traumatic Brain Injury. A Randomized Controlled Trial of a Family Intervention – Protocol and Pilot Study. In: Brain Injury. 2017.